“Heart Failure” is serious
But it doesn’t have to be as scary as it sounds.
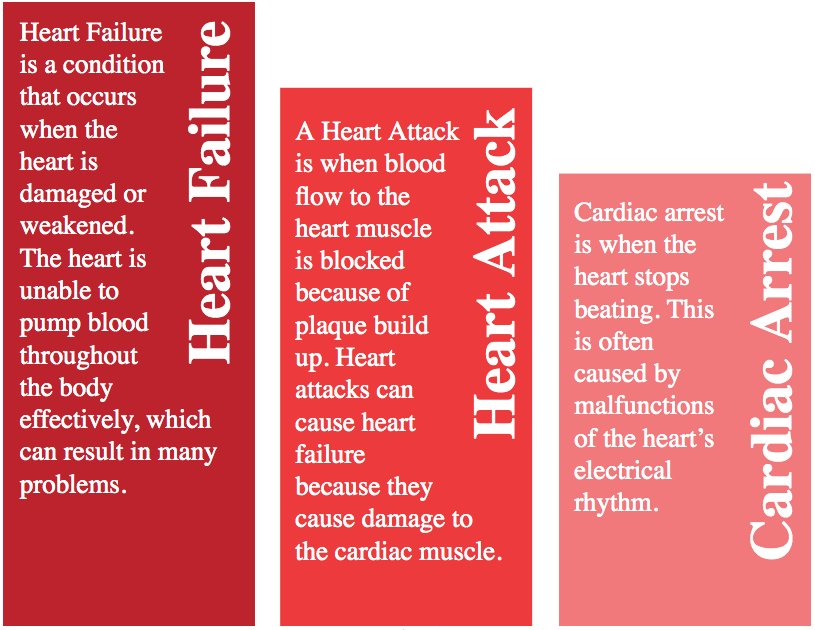
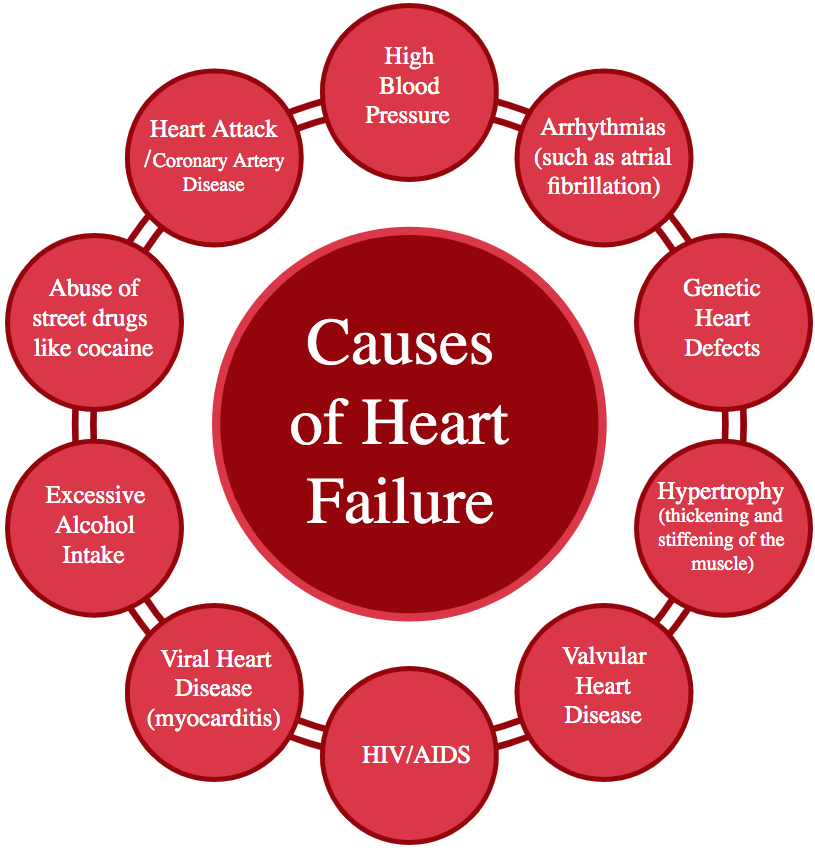
Heart failure doesn't mean the heart has "failed" or that it has stopped working. Instead, heart failure (CHF) means the heart isn’t pumping as well as it should. If you have been diagnosed with congestive heart failure, your quality of life and even your longevity can dramatically improve with early intervention. The sooner you start taking care of yourself and start following CHF lifestyle and medical recommendations, the longer and healthier a life you can hope to enjoy.


 1.jpg)